Sounding the Alarm on Alert Fatigue
 Ovayo Swartbooi
Ovayo Swartbooi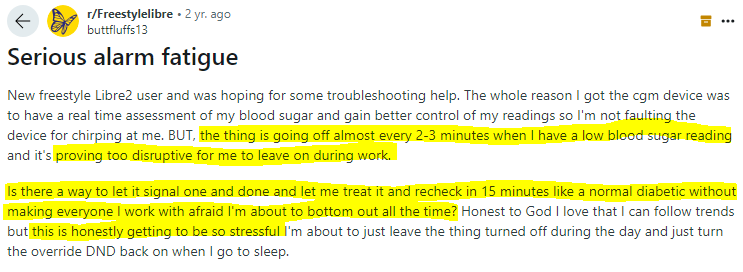
I can't recall the number of times I’ve wanted to throw a patient monitor out the window 😂
We are wired for action. The perception-action cycle—sensing, predicting, acting, and adjusting—highlights how the brain readily responds to the outside world, and acts accordingly. But what happens when this cycle is overwhelmed by a flood of alerts and alarms? Alert Fatigue
Where I worked, it was common practice to mute the monitors in ED. The sheer volume and frequency of alerts were unbearable. Now imagine them going off in unison at 3 a.m in the wards. Poor patients would dread the blaring of low battery alarms from those portable BP monitors. Yho! The noise was unrelenting. We all felt a sense of alert fatigue.
The situation is so bad that the American Society of Anaesthesiology released a statement on alarm management stating,
“Anesthesia professionals should not indefinitely silence or disable alarms on any device, unless [if] … (a) the device or module is not in use, (b) the device or module has malfunctioned (in this case, the device should not be used again until fully functional), or (c) the alarm is not relevant to the patient’s medical condition and supports using the AUDIO OFF or ALARM OFF modes. The alarm volume should be adjusted to an audible level factoring in the noise level of the clinical setting and to not create additional distractions.”
Let me explain the differences between Alerts and Alarms:
Alarms are regulated, are time-sensitive and critical. A delay of even a few seconds can impact patient safety. In the U.S, the FDA oversees alarm management vendors, resulting in strict regulations that limit the number of vendors offering alarm notification.
Alerts by definition are not life-threatening, less time-sensitive, and are not always regulated by the FDA. They are generated by systems like EMRs and the lower regulatory barriers mean that developers can add alerting capabilities more easily than traditional alarm management systems.
But should you pay attention?
Studies show that excessive alerts can lead to patient harm, and that 40% of alert overrides related to medication were clinically inappropriate.
Yikes! 👀
Here’s how UX designers can support the user
1. Create designs that prioritize alerts based on severity to prevent overwhelming users, and reduce alert fatigue.
2. Add clear feedback to ensures users understand the urgency of alerts
3. Differentiate between human error and technical faults. It helps to identify the best way to deal with and mitigate such issues. Think cybersecurity.
There’s still a lot of research to be done in this area. But it's clear that by simply improving usability and sticking to user-centered design principles, we can alleviate many of the stressors on our healthcare professionals.
One hopes we don’t start experiencing alert fatigue with wearables
… oh wait 😏
Subscribe to my newsletter
Read articles from Ovayo Swartbooi directly inside your inbox. Subscribe to the newsletter, and don't miss out.
Written by

Ovayo Swartbooi
Ovayo Swartbooi
🏥👩🏽⚕️Digital Health Consultant, Community Builder, SDG 3 and 9. 💡💭Emerging thought leader on Digital Health in Africa. 🌍I educate the world on how digital innovation can drive the delivery of value-based care on the African continent.