Article Review: Artificial intelligence powered coronary artery disease diagnosis from SPECT myocardial perfusion imaging a comprehensive deep learning study
 Aldo Yang
Aldo Yang3 min read
Objectives
- Developed deep learning (DL) models for automated coronary artery disease (CAD) diagnosis using single-photon emission computed tomography myocardial perfusion imaging (SPECT-MPI) polar maps.
- Compared various training strategies, including supervised, semi-supervised, and transfer learning, with different input types (rest, stress, early fusion, and late fusion).
- Evaluated models' performance in two tasks: (1) automating expert reader (ER) diagnosis and (2) predicting invasive coronary angiography (ICA)-based diagnosis.
- Demonstrated that combining data with and without ICA, along with semi-supervised learning, can improve DL model performance.
Methodology
- Implemented 13 different convolutional neural network (CNN) models, including CNN1, CNN2, DenseNet (121, 169, 201), EfficientNet (B0, B3), InceptionResNetV2, InceptionV3, ResNet (101V2, 152V2, 50V2), and VGG19.
- Used quantitative perfusion SPECT (QPS) to extract polar maps of rest and stress states.
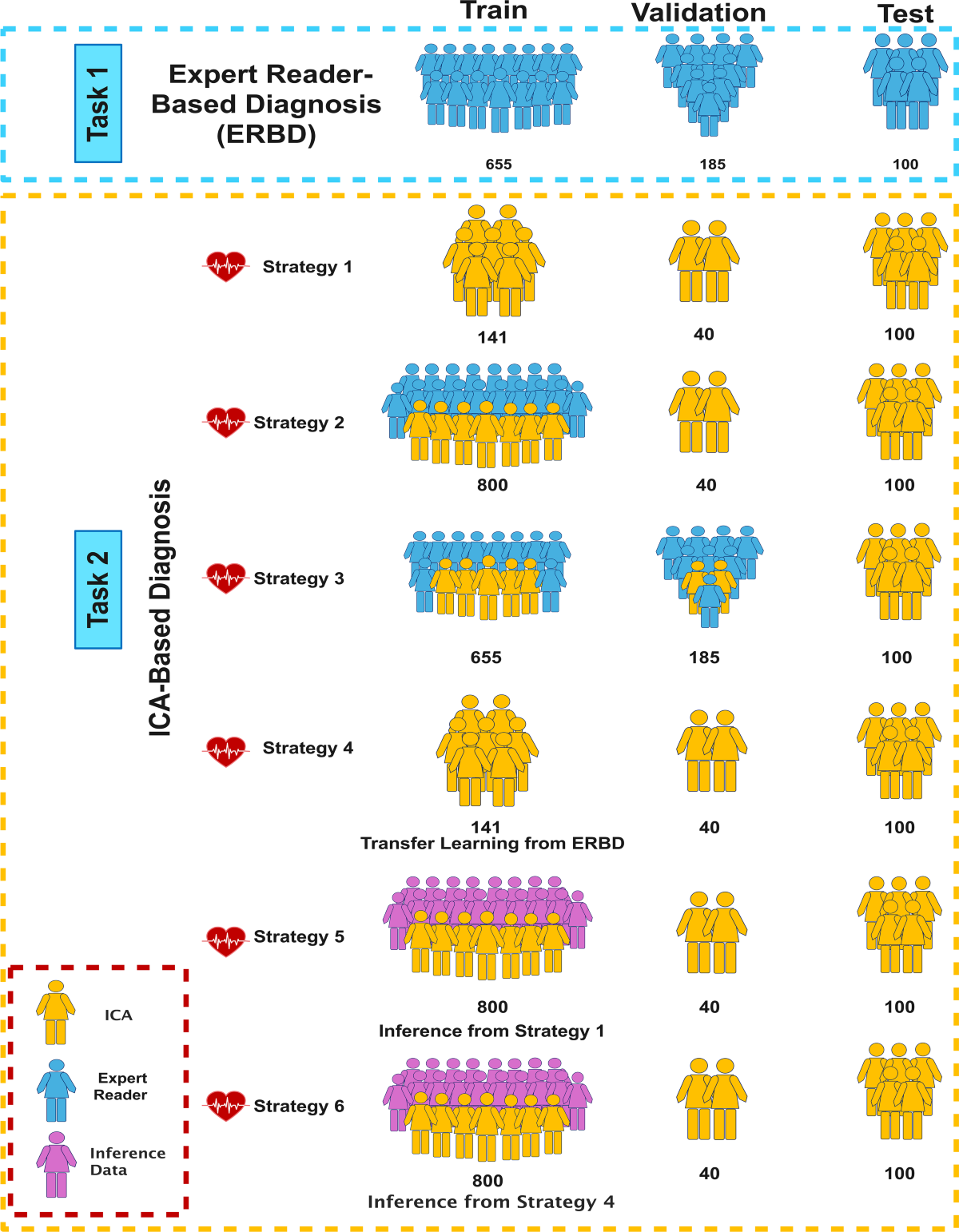
- Defined two tasks: (1) automated CAD diagnosis with ER assessment of SPECT-MPI as reference, and (2) CAD diagnosis from SPECT-MPI based on reference ICA reports.
- In Task 2, used six strategies for training DL models, including combinations of ER- and ICA-based diagnoses, and semi-supervised learning.
- Utilized four input types: rest polar maps, stress polar maps, early fusion (two-channel images of stress and rest), and late fusion (separate stress and rest inputs with 2D spatial pyramid pooling (SPP)).
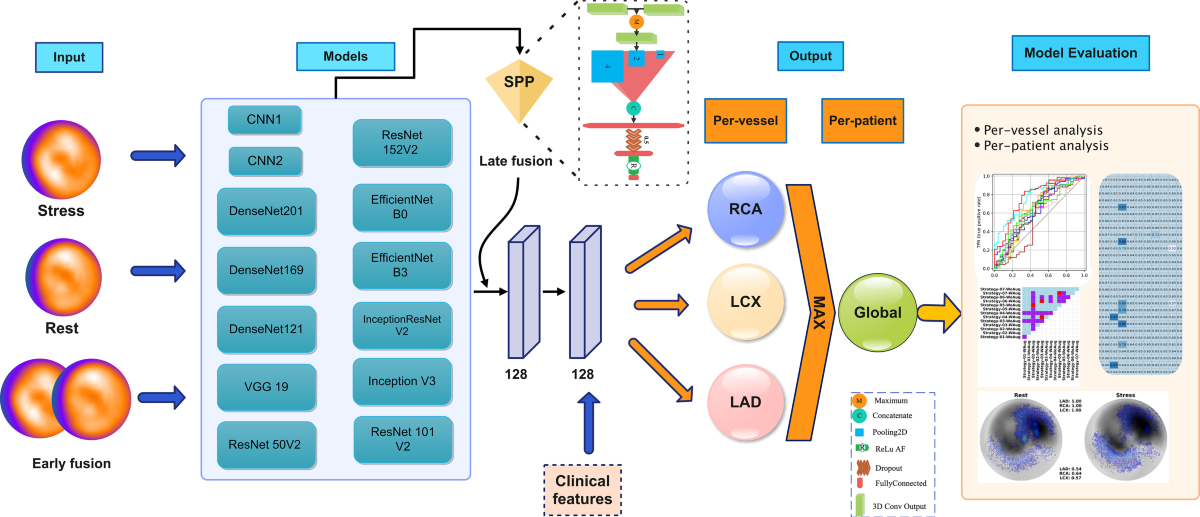
- Incorporated data augmentation (±10° rotations) and clinical features (age, gender, weight, height).
Results
- In Task 1 (ER-based diagnosis), the best models achieved AUCs of 0.89 (DenseNet201 Late Fusion) in per-vessel analysis and 0.83 (ResNet152V2 Late Fusion) in per-patient analysis.
- In Task 2 (ICA-based diagnosis), the best models achieved AUCs of 0.71 (Strategy 3, WoAug InceptionResNetV2 EarlyFusion) in per-vessel analysis and 0.77 (Strategy 5, WoAug ResNet152V2 EarlyFusion) in per-patient analysis.
- Statistical tests (DeLong and Wilcoxon rank sum) showed significant differences between models and strategies.
- The best DL model in per-patient analysis (Strategy 5 WoAug ResNet152V2 EarlyFusion) outperformed the expert reader's SS-based diagnosis in LAD (AUC: 0.80 vs. 0.58) and improved the new ER's performance with DL assistance (AUC: 0.68).
Discussions
- The study is comprehensive, exploring numerous DL models and training strategies. However, the sample size with ICA as the gold standard is relatively small (n=281). While the authors address this by incorporating ER-based diagnoses, the inherent subjectivity of ER assessments introduces a potential bias.
- The rationale for choosing specific DL architectures (CNN1, CNN2) is not clearly explained. Providing more details on the design choices would strengthen the methodology.
- The study uses a ±6-month window between SPECT and ICA. This could be a limitation, as disease progression might occur within this timeframe. A shorter interval would be preferable.
- While saliency maps are presented, their interpretation and clinical utility are not thoroughly discussed.
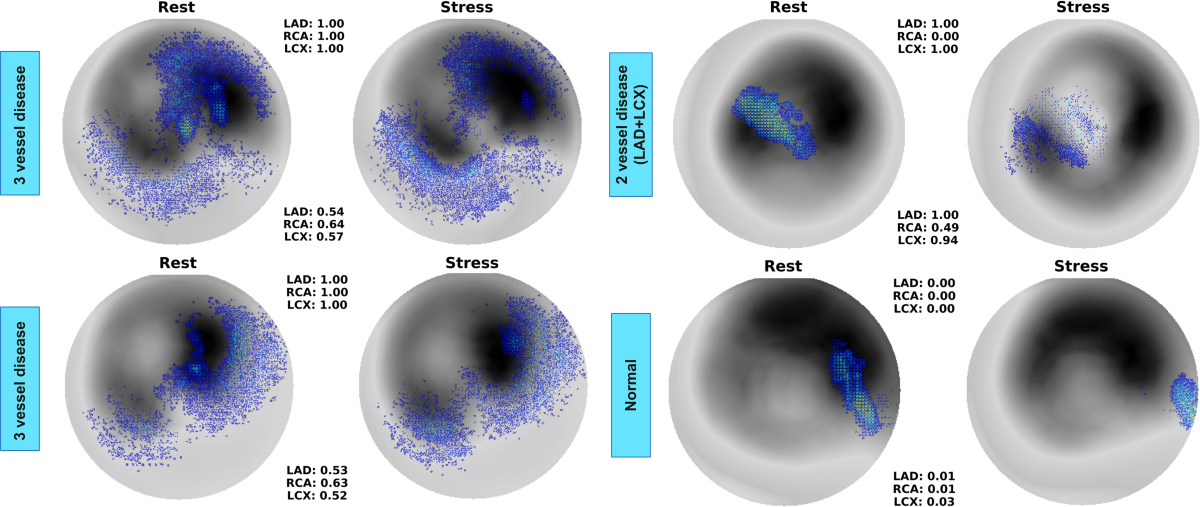 A more detailed analysis of how these maps correlate with specific angiographic findings would be valuable.
A more detailed analysis of how these maps correlate with specific angiographic findings would be valuable. - The study lacks external validation. Testing the models on an independent dataset would significantly enhance the generalizability of the findings.
0
Subscribe to my newsletter
Read articles from Aldo Yang directly inside your inbox. Subscribe to the newsletter, and don't miss out.
Written by
