CareMorph: AI-Powered Evolution in Digital Health Monitoring
 Venkata Krishna Azith Teja Ganti
Venkata Krishna Azith Teja Ganti
Abstract
The convergence of artificial intelligence (AI) and digital health has brought about a transformative wave in healthcare delivery, with "CareMorph" emerging as a conceptual paradigm for the dynamic, AI-driven evolution of health monitoring systems. This article explores the foundational technologies, benefits, challenges, and future prospects of CareMorph—a model wherein AI adapts, personalizes, and evolves with patient needs, healthcare environments, and clinical goals. Through real-time analytics, predictive modeling, and continuous learning, CareMorph represents a significant leap from static monitoring to intelligent, context-aware digital care ecosystems.
1. Introduction
In recent years, digital health technologies have evolved rapidly, yet much of their implementation remains reactive and limited to static data collection. CareMorph redefines this approach by infusing AI into the core of digital health monitoring systems, enabling continuous adaptation to individual patient trajectories. This AI-powered transformation facilitates more nuanced care interventions, personalized treatment strategies, and predictive health management.
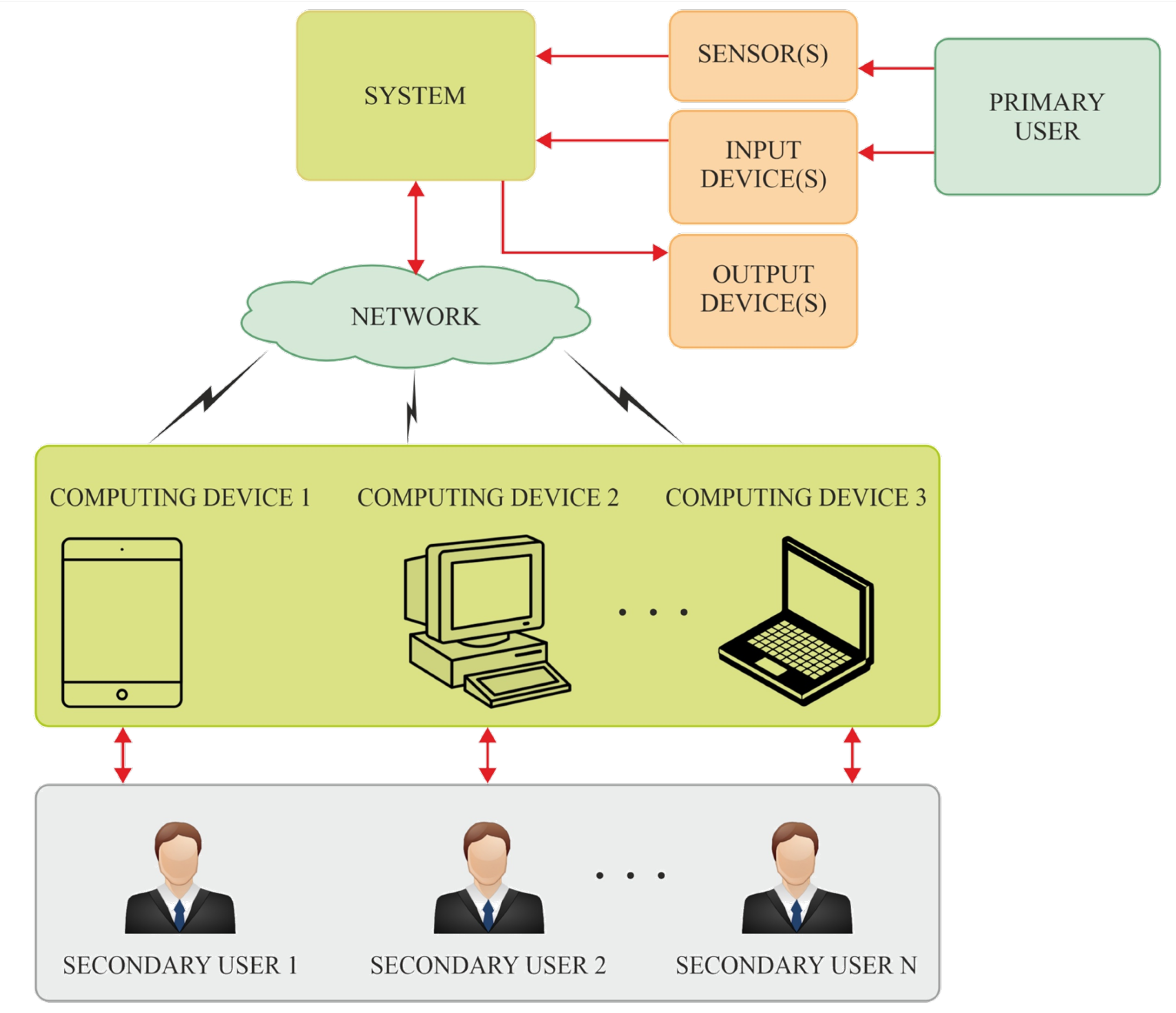
CareMorph is not a specific product but a conceptual framework or system architecture wherein AI morphs digital health monitoring to meet dynamically changing patient needs. It reflects the shift from device-centric data collection to intelligence-centered care delivery.
2. Core Technologies Behind CareMorph
CareMorph is underpinned by a constellation of AI technologies and connected systems. The key enablers include:
a. Machine Learning and Predictive Analytics:
Machine learning (ML) models in CareMorph systems analyze multi-dimensional patient data—vital signs, activity levels, speech patterns, sleep metrics—to detect patterns that precede clinical deterioration or improvement. For example, recurrent neural networks (RNNs) and transformer models help predict events like cardiac arrest, diabetic complications, or mental health crises before they manifest.
b. Edge Computing and IoT Integration:
Wearable devices and home-based sensors form the physical infrastructure of CareMorph. Through edge computing, data processing is decentralized, reducing latency and enhancing privacy. AI models deployed on edge devices can perform real-time assessments and alert both patients and clinicians.
c. Natural Language Processing (NLP):
CareMorph utilizes NLP to process electronic health records (EHRs), clinician notes, and patient-reported outcomes. This enables a holistic understanding of health contexts, social determinants of health, and subjective symptom descriptions.
d. Federated Learning for Privacy:
To train AI models across distributed datasets without compromising patient privacy, CareMorph systems often implement federated learning. This decentralized model-building approach allows devices to collaboratively learn without sharing raw data, meeting stringent privacy and regulatory requirements.
3. Key Features and Functions
CareMorph introduces a number of features that distinguish it from traditional monitoring systems:
Adaptive Monitoring: Sensors and AI algorithms dynamically adjust data collection parameters based on real-time analysis. For example, a patient's heart rate and sleep data might be sampled more frequently during illness and less during stable periods.
Predictive Interventions: Rather than waiting for symptoms, CareMorph anticipates deteriorations, offering early alerts to caregivers or triggering automated interventions (e.g., dosage adjustments in connected insulin pumps).
Personalization: Each patient has a unique "digital phenotype." CareMorph learns these signatures over time to tailor alerts, recommendations, and therapy plans.
Context Awareness: AI considers contextual variables such as weather, emotional state (via vocal sentiment analysis), or medication adherence to provide a comprehensive health assessment.
Closed-Loop Feedback: CareMorph systems engage in continuous learning. Patient responses to treatments feed back into the system, enhancing future recommendations and model accuracy.
4. Applications in Clinical and Home Settings
CareMorph has applications across diverse healthcare environments:
a. Chronic Disease Management:
For conditions like diabetes, hypertension, and COPD, CareMorph enables remote monitoring with real-time alerts. AI models predict exacerbations based on patterns in vital signs, medication adherence, and environmental triggers.
Eq.1.Predictive Health Score

b. Postoperative and Rehabilitation Care:
Patients recovering from surgery or injury benefit from adaptive monitoring that reduces hospital stays. AI tracks progress and suggests personalized recovery pathways, modifying intensity based on feedback.
c. Mental Health Monitoring:
CareMorph systems analyze speech tone, facial expressions (via video), and activity levels to detect early signs of depression or anxiety. Interventions can be delivered digitally, such as AI-guided cognitive behavioral therapy prompts.
d. Geriatric and Palliative Care:
Older adults with complex comorbidities often experience fragmented care. CareMorph offers continuity by integrating biometric data with medication and behavior monitoring, improving quality of life and reducing emergency visits.

5. Benefits of the CareMorph Model
Proactive Care Delivery: CareMorph reduces reliance on episodic care, emphasizing early detection and prevention.
Improved Clinical Outcomes: Continuous, personalized feedback enhances treatment adherence and reduces avoidable hospitalizations.
Empowered Patients: With transparent insights into their own health data and AI-guided tools, patients play a more active role in managing their care.
Operational Efficiency: Healthcare systems benefit from reduced burden on staff, optimized resource utilization, and better triage decisions.
6. Challenges and Limitations
Despite its promise, CareMorph faces several hurdles:
a. Data Silos and Interoperability:
Integrating data from wearables, EHRs, and home sensors requires standardized protocols and interoperability frameworks.
b. Model Bias and Equity:
AI models risk perpetuating health disparities if trained on non-representative data. Continuous validation across diverse populations is critical.
c. Regulatory and Ethical Concerns:
AI-driven clinical decisions raise accountability questions. Clear regulatory guidelines and ethical oversight are essential.
Eq.2.Personalization via Bayesian Updating

d. User Adoption and Trust:
Patients and clinicians must trust the system. Transparent AI explanations (e.g., via Explainable AI techniques) help build confidence in recommendations.
7. Future Outlook and Research Directions
As digital health infrastructure matures, CareMorph may evolve in the following directions:
Multi-Modal Fusion: Combining visual, audio, physiological, and textual data for deeper insights into patient status.
AI-Driven Digital Twins: Creating real-time digital replicas of patients to simulate disease progression and test treatment scenarios virtually.
Behavioral Nudging: Integrating behavioral economics with AI to encourage healthier lifestyles through micro-interventions.
Human-AI Collaboration: Developing systems where clinicians and AI co-create care plans, blending intuition with data-driven insight.

8. Conclusion
CareMorph represents a transformative vision for digital health monitoring: one that is intelligent, adaptive, and deeply personalized. By merging AI with ubiquitous sensors, cloud computing, and clinical expertise, CareMorph offers a roadmap for proactive, equitable, and efficient healthcare. As challenges are addressed through innovation and policy, the CareMorph paradigm could define the next decade of digital medicine.
Subscribe to my newsletter
Read articles from Venkata Krishna Azith Teja Ganti directly inside your inbox. Subscribe to the newsletter, and don't miss out.
Written by
